Trametinib
Overview
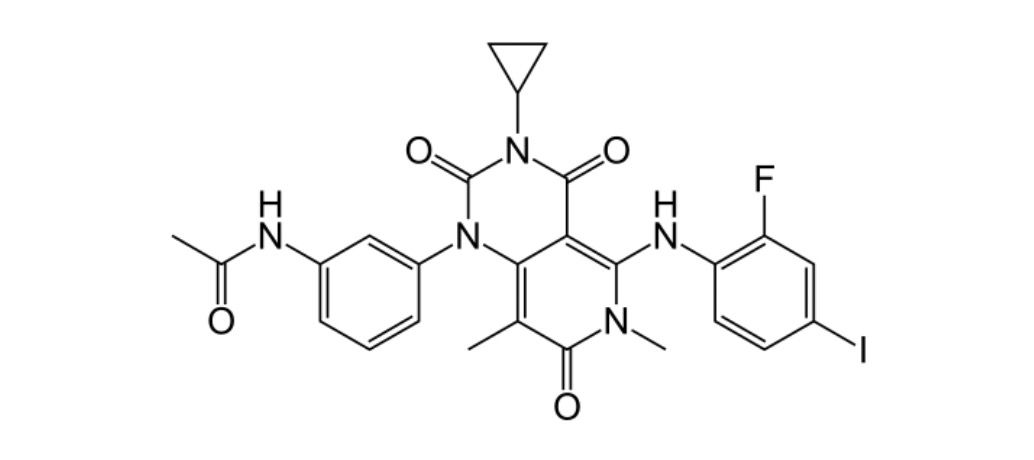
Trametinib is an oral selective inhibitor of MEK1 and MEK2, enzymes involved in the MAPK/ERK signaling pathway, which regulates cell proliferation and survival. It is primarily used in oncology for treating patients with unresectable or metastatic melanoma harboring BRAF V600E or V600K mutations. Trametinib is administered orally and is often combined with BRAF inhibitors to enhance efficacy and reduce resistance. The drug has demonstrated improvements in progression-free survival and overall survival in clinical trials. Key SEO terms include MEK inhibitor, targeted cancer therapy, melanoma treatment, BRAF mutation, oral oncology drug, and cancer pathway inhibition. Safety monitoring is essential to detect potential adverse events, and therapy should be supervised by oncology specialists.
Background and Date of Approval
Trametinib was developed as a selective MEK inhibitor to target aberrant signaling in cancers with MAPK pathway activation. By inhibiting MEK1/2, it blocks downstream ERK phosphorylation, reducing tumor cell proliferation. Trametinib received FDA approval in May 2013 for unresectable or metastatic melanoma with BRAF V600 mutations, and the EMA approved it shortly thereafter. The approval was based on pivotal clinical trials, including the METRIC study, which demonstrated significant improvement in progression-free survival compared with chemotherapy. Trametinib has since been incorporated into combination regimens with BRAF inhibitors such as dabrafenib, showing synergistic effects and improved patient outcomes. Its pharmacokinetics and safety profile have been extensively studied and reported in peer-reviewed literature.
Uses
Trametinib is indicated for patients with unresectable or metastatic melanoma carrying BRAF V600E or V600K mutations. It may be used as monotherapy in selected patients or in combination with BRAF inhibitors to prevent resistance and enhance clinical efficacy. Off-label use is occasionally considered in other cancers with MAPK pathway activation, but such use should be under specialist supervision. Treatment decisions are individualized, taking into account mutation status, disease stage, and patient health.
Administration
Trametinib is administered orally, with a recommended dose of 2 mg once daily, at least one hour before or two hours after a meal. Dose adjustments may be required for patients experiencing significant toxicity or adverse reactions. Monitoring of cardiac function, dermatologic events, and ocular toxicity is essential during therapy. Concomitant medications should be reviewed for potential interactions affecting Trametinib metabolism, primarily via CYP3A4 pathways.
Side Effects
Frequent side effects include rash, diarrhea, fatigue, edema, nausea, and stomatitis. Most adverse events are mild to moderate and manageable with supportive care. Patients are advised to report worsening symptoms promptly, as early intervention can prevent more serious complications. Oncology teams should provide guidance for managing common toxicities to maintain adherence and optimize outcomes.
Warnings
Serious adverse events associated with Trametinib include cardiomyopathy, retinal vein occlusion, interstitial lung disease, and severe dermatologic reactions. It is contraindicated in patients with known hypersensitivity to Trametinib or its excipients. Use during pregnancy is not recommended due to potential teratogenicity. Close monitoring for cardiac and ocular function, as well as early recognition of severe skin reactions, is critical to patient safety.
Precautions
Trametinib may interact with CYP3A4 inducers or inhibitors, affecting drug levels. Caution is advised in patients with pre-existing cardiac, ocular, or pulmonary conditions. Patients should be counseled on avoiding pregnancy and using effective contraception. Comprehensive monitoring and individualized dose adjustments are recommended to minimize toxicity while maintaining therapeutic efficacy.
Expert Tips
Prescribers should confirm BRAF mutation status before initiating Trametinib and consider combination therapy with a BRAF inhibitor for eligible patients. Pharmacists can assist with counseling on proper oral administration, managing drug interactions, and monitoring for adverse events. Education on recognizing early signs of cardiotoxicity, ocular complications, and dermatologic reactions is essential. Collaborative care and regular follow-up optimize both safety and clinical outcomes.