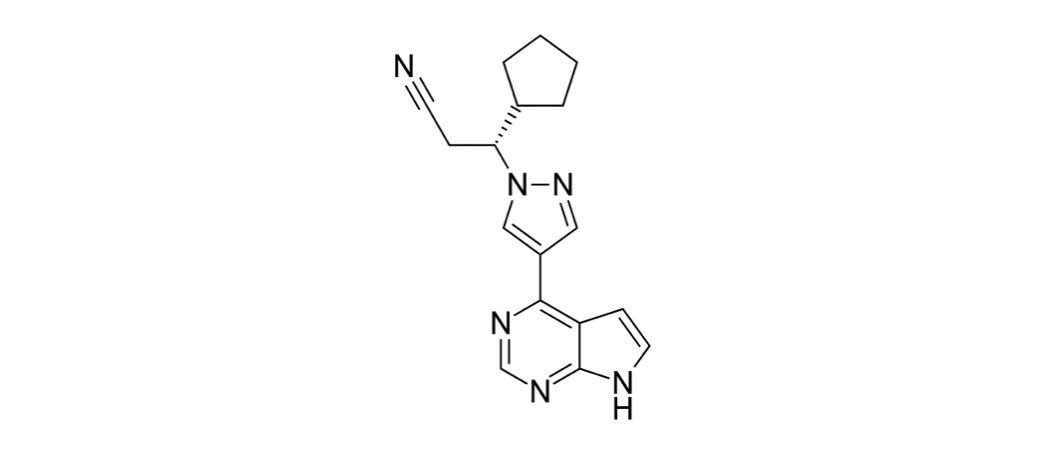
Ruxolitinib
Overview
Ruxolitinib is a small-molecule Janus kinase inhibitor that selectively targets JAK1 and JAK2, key enzymes involved in cytokine signaling, immune regulation, and blood cell production. By inhibiting these pathways, ruxolitinib reduces abnormal inflammatory signaling and excessive proliferation of blood cell precursors seen in certain hematologic and immune-mediated diseases. It is administered primarily as an oral tablet and is clinically important for improving symptom burden, controlling splenomegaly, and modulating immune-driven tissue injury in appropriate patients. Ruxolitinib represents a targeted therapeutic approach rather than cytotoxic chemotherapy, but its effects on immune and hematopoietic pathways require structured monitoring. Clinical benefit depends on appropriate patient selection, dose adjustment based on laboratory parameters, and ongoing assessment of infection risk.
Background and Date of Approval
Ruxolitinib was developed following the identification of JAK-STAT pathway dysregulation in myeloproliferative neoplasms. It received initial regulatory approval from the United States Food and Drug Administration in 2011 for the treatment of intermediate- or high-risk myelofibrosis. Subsequent approvals expanded its use to patients with polycythemia vera who are resistant to or intolerant of hydroxyurea. Additional approvals were granted for steroid-refractory acute graft-versus-host disease in 2019 and chronic graft-versus-host disease in 2021. European and other international regulatory agencies have approved ruxolitinib for similar indications based on large randomized clinical trials demonstrating symptom control and disease-related benefit.
Uses
Ruxolitinib is indicated for the treatment of intermediate- or high-risk myelofibrosis to reduce splenic enlargement and disease-related symptoms. It is also approved for polycythemia vera in patients who have an inadequate response to or cannot tolerate hydroxyurea. In transplant medicine, ruxolitinib is used for steroid-refractory acute graft-versus-host disease and for chronic graft-versus-host disease after failure of prior systemic therapy. It may be used as monotherapy or alongside other supportive or immunosuppressive treatments depending on the clinical setting.
Administration
Ruxolitinib is administered orally, typically twice daily, with or without food. Initial dosing depends on the indication and baseline platelet counts, particularly in myelofibrosis and polycythemia vera. In graft-versus-host disease, lower starting doses may be used with gradual escalation based on response and tolerability. Dose adjustments are commonly required in response to cytopenias, hepatic or renal impairment, or drug interactions. Treatment duration is individualized and guided by clinical benefit and laboratory monitoring.
Side Effects
Common side effects of ruxolitinib include anemia, thrombocytopenia, and neutropenia related to suppression of bone marrow activity. Patients may also experience headache, dizziness, fatigue, gastrointestinal symptoms such as nausea or diarrhea, weight gain, and peripheral edema. Mild infections and skin reactions have also been reported. Side effects vary between individuals and are often manageable with dose modification and regular medical supervision.
Warnings
Serious adverse events associated with ruxolitinib include severe cytopenias, serious bacterial, viral, or fungal infections, and reactivation of latent infections. There is an increased risk of bleeding in patients with significantly reduced platelet counts. Rare cases of secondary malignancies have been reported in association with long-term immunosuppression. Abrupt discontinuation may lead to rapid symptom recurrence or disease flare, and treatment interruption should be managed carefully under medical guidance.
Precautions
Baseline evaluation before starting ruxolitinib should include complete blood counts and assessment of liver and kidney function. Caution is required in patients with active infections, prior history of opportunistic infections, or significant organ impairment. Concomitant use of strong CYP3A4 inhibitors can increase ruxolitinib exposure and may require dose reduction. Live vaccines are generally avoided during treatment due to immunosuppressive effects. Ongoing monitoring is essential throughout therapy.
Expert Tips
Ensure baseline and periodic blood count monitoring is in place before initiating ruxolitinib. Educate patients about infection risk and the importance of reporting fever or new symptoms promptly. Adjust doses proactively in response to declining blood counts rather than waiting for severe toxicity. Coordinate care when ruxolitinib is used alongside other immunosuppressive therapies, and counsel patients against abrupt discontinuation without medical advice.