Olaparib
Overview
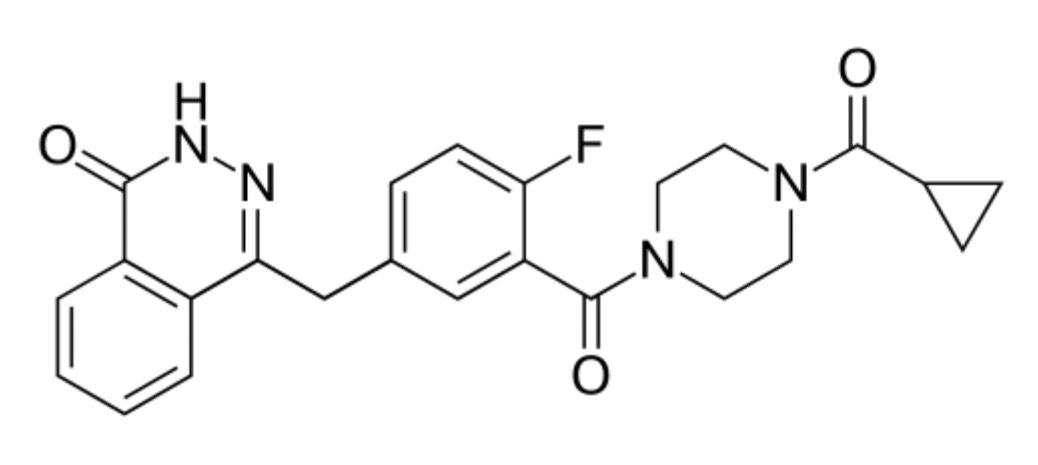
Olaparib is an oral poly (ADP-ribose) polymerase (PARP) inhibitor used as a targeted therapy in oncology. It works by blocking PARP enzymes involved in DNA repair, making cancer cells with BRCA1 or BRCA2 mutations more vulnerable to cell death. Olaparib has transformed the management of ovarian cancer, breast cancer, pancreatic cancer, and prostate cancer, especially in patients with germline or somatic BRCA mutations. It is administered orally in tablet form, typically in combination with other therapies or as maintenance therapy following platinum-based chemotherapy. Known by its brand name Lynparza, olaparib has demonstrated strong efficacy in prolonging progression-free survival in patients with advanced malignancies. Its targeted approach makes it a key part of personalized medicine in oncology.
Background and Date of Approval
Olaparib was developed as the first-in-class PARP inhibitor and marked a significant milestone in precision oncology. The United States Food and Drug Administration (FDA) first approved olaparib in December 2014 for the treatment of advanced ovarian cancer in patients with deleterious or suspected BRCA mutations who had received at least three prior lines of chemotherapy. Subsequent approvals expanded its use to include maintenance treatment for recurrent ovarian cancer, metastatic HER2-negative breast cancer with germline BRCA mutations, pancreatic cancer, and metastatic castration-resistant prostate cancer with homologous recombination repair gene mutations. The European Medicines Agency (EMA) also granted approval in 2014, with progressive label expansions in later years. Clinical studies such as SOLO-1, SOLO-2, and PROfound provided pivotal evidence supporting its use, showing meaningful survival benefits in BRCA-mutated cancers. Its mechanism of synthetic lethality, achieved by inhibiting DNA repair in tumor cells while sparing normal cells, represents a paradigm shift in cancer treatment.
Uses
Olaparib is indicated for multiple cancers driven by defective DNA repair mechanisms. In ovarian cancer, it is used as maintenance therapy in patients with recurrent disease who have responded to platinum-based chemotherapy. In breast cancer, olaparib is approved for HER2-negative metastatic disease in patients with germline BRCA mutations. In pancreatic cancer, it is used as maintenance therapy for patients with germline BRCA mutations whose disease has not progressed after at least 16 weeks of platinum-based chemotherapy. In prostate cancer, olaparib is indicated for metastatic castration-resistant prostate cancer with deleterious or suspected homologous recombination repair gene mutations. Off-label, it has been studied in other tumor types where DNA repair deficiencies play a critical role.
Administration
Olaparib is administered orally, with tablets taken twice daily. The recommended starting dose is 300 mg taken twice daily, with or without food. Dosing adjustments may be necessary based on side effects, kidney or liver function, or concomitant medications. Treatment is continued until disease progression or unacceptable toxicity occurs. Close monitoring is required for hematologic parameters, particularly in patients at risk of anemia, neutropenia, or thrombocytopenia.
Side Effects
The most frequently reported side effects of olaparib include nausea, fatigue, vomiting, diarrhea, decreased appetite, dysgeusia, anemia, and abdominal pain. Patients may also experience cough, musculoskeletal pain, or elevations in serum creatinine. Side effects often occur early in treatment but may improve with supportive care or dose modification. Fatigue and gastrointestinal disturbances remain among the most bothersome symptoms affecting quality of life.
Warnings
Serious risks of olaparib include myelodysplastic syndrome and acute myeloid leukemia, though these occur rarely. Pneumonitis is another uncommon but serious adverse event requiring discontinuation. Embryo-fetal toxicity has been observed, and use in pregnancy is contraindicated. Olaparib should not be combined with strong CYP3A inhibitors or inducers without appropriate dose adjustments. Patients with renal or hepatic impairment require special consideration.
Precautions
Patients receiving olaparib should be monitored regularly for blood counts and signs of infection or bleeding. Concomitant use of drugs affecting CYP3A metabolism may alter olaparib exposure, requiring careful management. Grapefruit and Seville oranges should be avoided during therapy due to their CYP3A inhibitory effects. Women of childbearing potential should use effective contraception during and for at least one month after treatment. Men with female partners of reproductive potential should also use effective contraception during and for three months after therapy. Breastfeeding is not recommended during treatment.
Expert Tips
Prescribers should ensure that BRCA mutation status or homologous recombination deficiency testing is confirmed before initiating olaparib therapy. Pharmacists should counsel patients on adherence, as missed doses can impact efficacy. Monitoring for anemia is critical, and patients may require supportive care with blood transfusions. Early management of nausea with antiemetics can improve compliance. Patient education about avoiding interacting drugs and foods is also key to ensuring safety and therapeutic effectiveness.