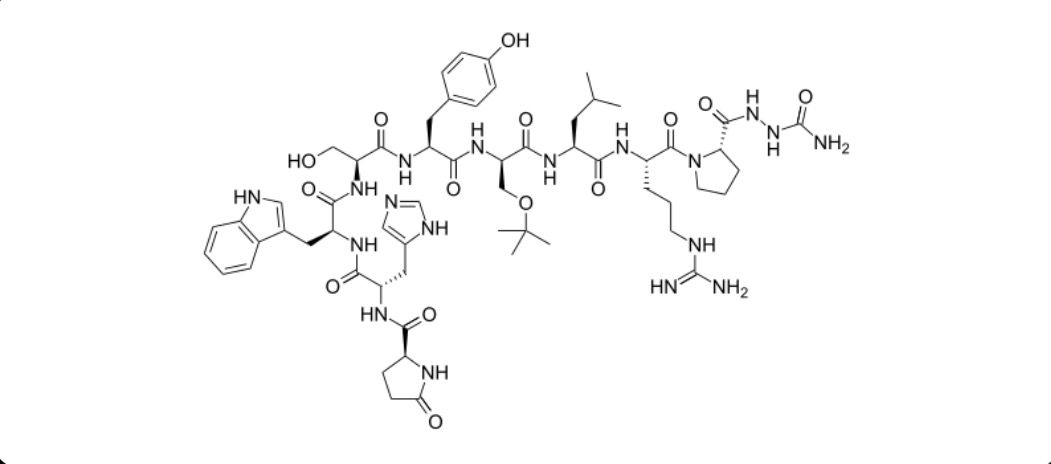
Goserelin Acetate
Overview
Goserelin acetate is a synthetic analogue of luteinizing hormone-releasing hormone that acts on the pituitary gland to regulate sex hormone production. After initial stimulation, continued administration suppresses the release of luteinizing hormone and follicle-stimulating hormone, leading to a marked reduction in testosterone levels in men and estrogen levels in women. This hormonal suppression disrupts the growth of hormone-dependent tumors and reduces abnormal hormone-driven tissue activity. Goserelin acetate is administered as a long-acting subcutaneous implant that provides continuous drug release over a defined period. It is clinically important as a reversible, non-surgical method of achieving medical castration or ovarian suppression, allowing disease control while avoiding permanent surgical procedures. Careful monitoring is required to manage hormonal, metabolic, and skeletal effects during therapy.
Background and Date of Approval
Goserelin acetate was developed during the advancement of gonadotropin-releasing hormone analogues in the late twentieth century. It received regulatory approval from major authorities including the United States Food and Drug Administration for use in hormone-sensitive prostate cancer, followed by approvals for additional oncologic and gynecologic indications. Over time, regulatory agencies in Europe and other regions approved goserelin for estrogen receptor-positive breast cancer in premenopausal women, endometriosis, and uterine fibroids. Multiple dosing formulations were approved to allow monthly or extended-interval administration based on clinical need and indication.
Uses
Goserelin acetate is indicated for the treatment of hormone-sensitive prostate cancer to suppress testosterone production and slow disease progression. In women, it is used for estrogen receptor-positive breast cancer as part of ovarian suppression strategies, often in combination with other systemic therapies. It is also approved for the management of endometriosis and uterine fibroids, where reducing estrogen levels can alleviate symptoms and reduce tissue growth. Use may be temporary or long term depending on disease type, treatment goals, and patient response.
Administration
Goserelin acetate is administered as a subcutaneous depot implant, typically placed in the lower abdominal wall by a healthcare professional. The implant delivers medication continuously over a period of approximately one month or up to three months, depending on the formulation. Dosing schedules vary by indication and patient characteristics. Treatment duration is individualized and guided by therapeutic response, tolerability, and long-term management considerations. Adherence to scheduled implant administration is essential to maintain effective hormone suppression.
Side Effects
Common side effects of goserelin acetate are related to reduced sex hormone levels and include hot flashes, sweating, decreased libido, sexual dysfunction, mood changes, headache, and fatigue. Local reactions at the injection site such as pain, bruising, or redness may occur. In women, menstrual irregularities or amenorrhea are common, while prolonged therapy in all patients may contribute to loss of bone mineral density. Side effects vary between individuals and are often manageable with clinical support.
Warnings
Serious adverse events associated with goserelin acetate include significant bone density loss with prolonged use, increasing the risk of osteoporosis and fractures. Cardiovascular events and metabolic changes have been reported in some patients undergoing long-term hormonal suppression. Severe allergic reactions are rare but possible. Goserelin is contraindicated in pregnancy due to the risk of fetal harm, and caution is required in patients with existing cardiovascular disease, diabetes, or osteoporosis.
Precautions
Baseline assessment before starting goserelin acetate should include evaluation of bone health, cardiovascular risk factors, and relevant metabolic parameters. Ongoing monitoring is recommended during treatment, especially in patients receiving long-term therapy. Drug interactions are generally limited due to the peptide nature of the molecule, but concurrent treatments affecting hormonal or metabolic pathways should be reviewed. Effective contraception should be discussed when pregnancy prevention is required.
Expert Tips
Educate patients about the expected hormonal effects and the timeline for symptom changes after initiation of therapy. Ensure consistent scheduling of depot implant administration to maintain hormone suppression. Monitor bone health and consider preventive strategies such as calcium and vitamin D supplementation when appropriate. Coordinate multidisciplinary care for patients with significant comorbidities, and counsel patients to report cardiovascular symptoms, severe mood changes, or signs of skeletal complications promptly.