Dasatinib
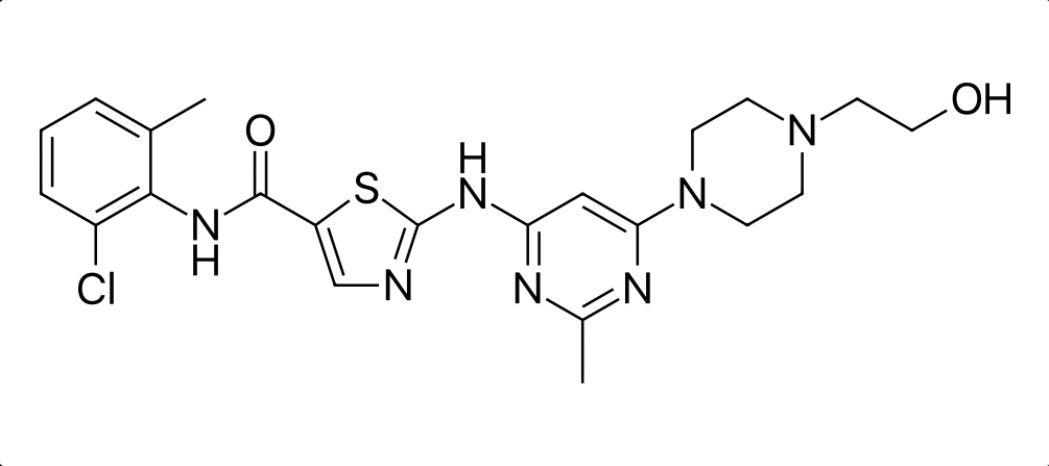
Overview
Dasatinib is an orally administered small‑molecule tyrosine kinase inhibitor that targets the BCR‑ABL fusion protein and multiple Src family kinases, which are abnormally active in certain leukemias. By inhibiting these kinases, dasatinib interferes with signals that promote proliferation and survival of malignant white blood cells, making it a key targeted therapy in selected blood cancers. Its mechanism differs from earlier agents by having broader inhibitory activity against both active and inactive conformations of BCR‑ABL and by inhibiting additional kinases involved in disease progression and resistance. Dasatinib is used primarily in Philadelphia chromosome‑positive chronic myeloid leukemia across disease phases and in Philadelphia chromosome‑positive acute lymphoblastic leukemia, including cases resistant or intolerant to prior therapy. Its oral administration allows for outpatient dosing, but it requires careful clinical monitoring due to potential effects on blood counts, cardiac function, and other organ systems. Dasatinib’s role in modern oncology reflects its utility in managing kinase‑driven leukemias, particularly where resistance to first‑line therapy has developed.
Background and Date of Approval
Dasatinib was developed as a second‑generation tyrosine kinase inhibitor to address resistance and intolerance to earlier therapies in chronic myeloid leukemia. It received initial regulatory approval from the United States Food and Drug Administration in June 2006 for the treatment of adults with Philadelphia chromosome‑positive chronic myeloid leukemia and Philadelphia chromosome‑positive acute lymphoblastic leukemia who were resistant or intolerant to prior therapy. In October 2010, dasatinib was approved by the FDA for newly diagnosed adults with Philadelphia chromosome‑positive chronic myeloid leukemia in chronic phase. Later, in November 2017, the FDA expanded approval to include pediatric patients with Philadelphia chromosome‑positive chronic myeloid leukemia in chronic phase. Regulatory agencies in numerous other countries, including the European Medicines Agency, have similarly authorised dasatinib for equivalent indications based on pivotal clinical trials demonstrating efficacy in chronic myeloid leukemia and acute lymphoblastic leukemia.
Uses
Dasatinib is indicated for the treatment of adult patients with newly diagnosed Philadelphia chromosome‑positive chronic myeloid leukemia in chronic phase. It is also indicated for adults with chronic, accelerated, or myeloid or lymphoid blast phase Philadelphia chromosome‑positive chronic myeloid leukemia who are resistant or intolerant to prior therapy. In addition, dasatinib is indicated for adults with Philadelphia chromosome‑positive acute lymphoblastic leukemia with resistance or intolerance to prior therapy. Pediatric indications include treatment of Philadelphia chromosome‑positive chronic myeloid leukemia and newly diagnosed Philadelphia chromosome‑positive acute lymphoblastic leukemia in combination with chemotherapy for patients aged one year and older.
Administration
Dasatinib is administered orally as a tablet. For adults with chronic phase chronic myeloid leukemia, the recommended starting dose is typically 100 mg once daily. For adults with accelerated or blast phase chronic myeloid leukemia and Philadelphia chromosome‑positive acute lymphoblastic leukemia, the recommended starting dose is generally 140 mg once daily. Pediatric dosing is based on body weight for younger patients. Dasatinib may be taken with or without food, and tablets should be swallowed whole without crushing or chewing. Treatment is continued until disease progression or unacceptable toxicity, with routine monitoring of blood counts and clinical status guiding ongoing dosing decisions.
Side Effects
Common side effects seen with dasatinib include low blood cell counts such as thrombocytopenia, neutropenia, and anemia, gastrointestinal symptoms such as diarrhea and nausea, fatigue, headache, skin rash, and fluid retention including peripheral edema. Patients may also experience cough, muscle pain, and weight changes. The severity and types of side effects can vary among individuals and are typically managed with supportive care, dose adjustments, or temporary treatment interruption under medical supervision.
Warnings
Dasatinib is associated with serious adverse events including significant myelosuppression, which can lead to severe thrombocytopenia and neutropenia, increased risk of bleeding, and serious infections. It can also cause pulmonary arterial hypertension, pleural effusion, and cardiac complications including QT prolongation. Severe fluid retention and gastrointestinal complications have been reported. Dasatinib is harmful during pregnancy and contraindicated in pregnancy due to potential teratogenic effects, and effective contraception should be maintained during treatment. Treatment interruption or discontinuation is required in cases of life‑threatening toxicity.
Precautions
Before initiating dasatinib, baseline assessments including complete blood counts, liver function tests, and cardiac evaluation are advised. Caution is required in patients with pre‑existing cardiovascular or pulmonary conditions. Dasatinib is metabolised by hepatic enzymes, and concomitant use of strong CYP3A4 inhibitors or inducers can significantly alter plasma concentrations, necessitating dose adjustments or alternative therapy. Concomitant use with drugs that may prolong the QT interval should be avoided or closely monitored. Dasatinib should not be used during pregnancy or breastfeeding due to potential harm to the fetus or infant. Regular monitoring for cytopenias, organ dysfunction, and clinical signs of serious toxicities helps mitigate risks.
Expert Tips
When prescribing dasatinib, assess the patient’s baseline hematologic status, cardiovascular history, and concomitant medications to optimise safety. Provide detailed counselling on administration, emphasizing that the tablet should be swallowed whole and may be taken with or without food. Monitor complete blood counts frequently during the initial months of therapy and periodically thereafter, along with regular assessment of blood pressure and cardiac status. Educate patients to report symptoms such as unusual bleeding, shortness of breath, chest pain, or new neurologic symptoms promptly. Coordinate care with supportive treatments and consider dose modifications for adverse events to maintain therapeutic benefit while minimising toxicity.