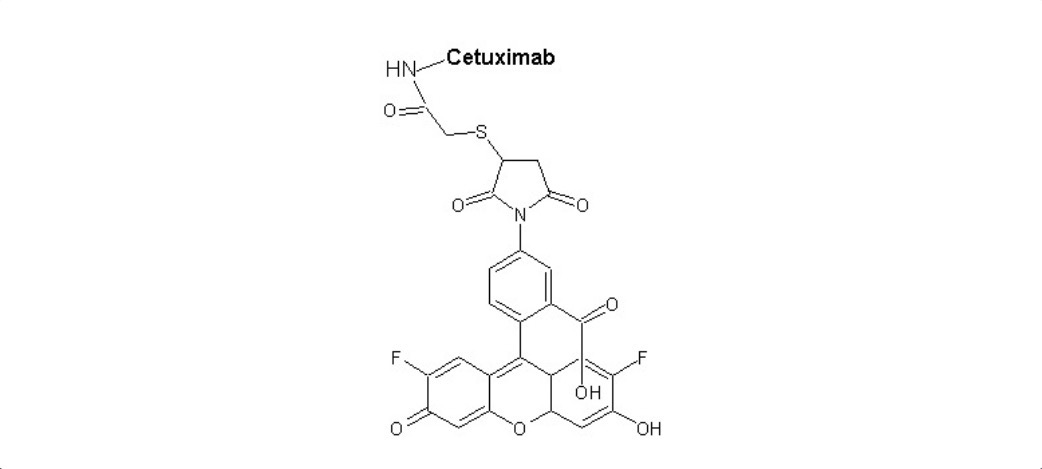
Cetuximab
Overview
Cetuximab is a chimeric (mouse/human) IgG1 monoclonal antibody that binds specifically to the epidermal growth factor receptor (EGFR) on the surface of cancer cells. By blocking ligand binding and downstream signaling, Cetuximab inhibits cell proliferation, angiogenesis, and survival of EGFR-expressing tumour cells. Cetuximab is administered by intravenous infusion and is indicated for treatment of metastatic colorectal cancer in patients whose tumours are wild-type for KRAS and for squamous cell carcinoma of the head and neck, either in combination with other therapies or as monotherapy after failure of other treatments. Cetuximab’s clinical benefit is most pronounced when tumour profiling confirms absence of specific KRAS mutations.
Background and Date of Approval
Cetuximab was approved by the U.S. Food and Drug Administration in 2004, initially for use in EGFR-expressing metastatic colorectal cancer patients who had failed standard chemotherapy consisting of irinotecan and oxaliplatin. Since then, regulatory approval has expanded to include use in combination with FOLFIRI as a first-line option for KRAS wild-type metastatic colorectal cancer, use in squamous cell carcinoma of the head and neck in combination with radiation therapy or with platinum-based chemotherapy, and as monotherapy in certain recurrent or metastatic settings. The European Medicines Agency also includes similar indications under its product information. Major clinical trials such as CRYSTAL, EXTREME, BOND, and others established efficacy in survival, progression-free survival, and tumour response, especially in patients confirmed as KRAS wild-type.
Uses
Cetuximab indications include treatment of metastatic colorectal cancer in combination with FOLFIRI for first-line therapy in patients with KRAS wild-type, use in combination with irinotecan in patients who are refractory to prior irinotecan-based therapy, and as monotherapy in those who are intolerant to or have failed oxaliplatin- and irinotecan-based regimens. In head and neck cancer, Cetuximab is used in combination with radiation for locally or regionally advanced disease, in recurrent or metastatic disease with platinum-based chemotherapy, and as a single agent for patients whose prior therapy has failed. Determination of tumour KRAS mutational status is required for colorectal cancer, as only wild-type KRAS patients derive benefit; use is not indicated for patients with known KRAS or RAS mutations.
Administration
Cetuximab is administered via intravenous infusion. The initial loading dose is 400 mg/m² infused over approximately 120 minutes, followed by maintenance doses of 250 mg/m² given weekly as a 60-minute infusion. In some settings dose schedule modifications may apply. Before first dose, premedication with antihistamines (and sometimes corticosteroids) is often given to reduce risk of infusion reactions. Treatment continues until disease progression or unacceptable toxicity. Regular monitoring is necessary for infusion reactions, skin toxicities, and electrolyte disturbances.
Side Effects
Patients commonly experience skin reactions such as acneiform rash, dry skin, itching, and paronychia. Other frequent side effects include diarrhea, fatigue, nausea, and low magnesium levels. Infusion reactions such as fever, chills or chills and rigors may occur especially with initial doses. Most side effects are manageable with supportive care, dose adjustments or temporary interruption.
Warnings
Cetuximab carries serious risks including severe infusion reactions, cardiopulmonary arrest, and interstitial lung disease in rare cases. Respiratory complications can occur. Patients may develop electrolyte disturbances (e.g., hypomagnesemia) which require correction; renal or cardiac impairment may exacerbate risk. Use in pregnancy is contraindicated unless clearly needed. There is a boxed warning for infusion reactions and cardiopulmonary events in the prescribing information.
Precautions
Cetuximab should be used only in patients with confirmed wild-type KRAS for colorectal cancer indication. Premedication to reduce infusion reactions is advised. Electrolyte levels—especially magnesium, potassium, and calcium—should be monitored before and during therapy. Care is needed when combining with other agents that increase risk for skin toxicity or with therapies that affect EGFR signaling. Renal or hepatic impairment may affect drug handling, so monitoring of organ function is recommended.
Expert Tips
Before prescribing, ensure KRAS mutational testing is done to avoid ineffective therapy. Counsel patients about skin care, sun protection, and recognizing early signs of rash and infection. Infusion should be administered by trained personnel with emergency support in place for infusion reactions. Pharmacists should review concomitant medications that may exacerbate toxicity and monitor electrolytes. Dose should be withheld or discontinued in the event of severe adverse reactions or hypersensitivity.