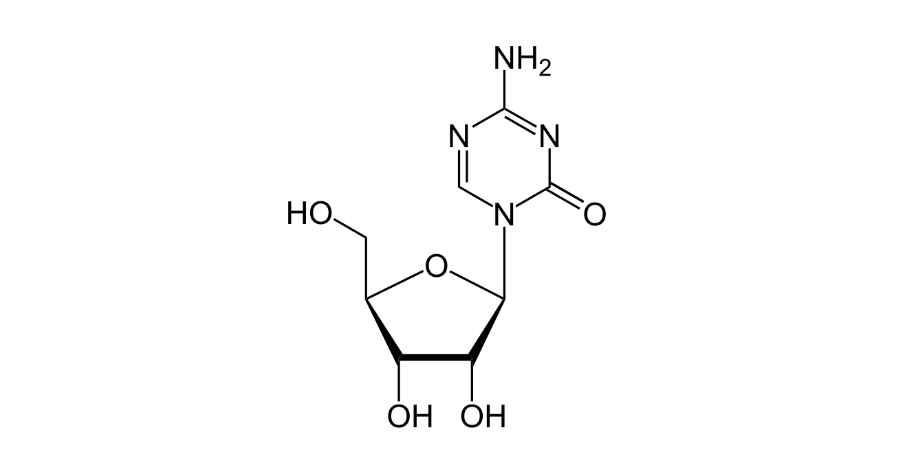
Azacitidine
Overview
Azacitidine is a cytidine analogue antineoplastic agent classified as a hypomethylating chemotherapy drug that interferes with DNA and RNA synthesis, leading to the death of rapidly dividing abnormal cells and restoration of normal hematopoiesis in certain bone marrow disorders. It is available as an injectable form administered under clinical supervision and an oral maintenance formulation used in specific leukemia settings. Through incorporation into nucleic acids, azacitidine inhibits DNA methyltransferase, causing hypomethylation of DNA and reactivation of tumor suppressor genes, with consequent inhibition of malignant cell proliferation and induction of apoptosis. Its mechanism of action distinguishes it from traditional cytotoxic agents by targeting epigenetic dysregulation, making it particularly useful in myelodysplastic syndromes, chronic myelomonocytic leukemia with specific marrow involvement, and acute myeloid leukemia in defined treatment sequences. Azacitidine’s role in hematologic oncology reflects both direct antitumor effects and modulation of malignant progenitor cell dynamics under a structured treatment regimen.
Background and Date of Approval
Azacitidine was first approved by the United States Food and Drug Administration on May 19, 2004 for the treatment of all subtypes of myelodysplastic syndromes, establishing a foundational therapy for these bone marrow failure disorders. Subsequent regulatory approvals have expanded its use in other hematologic indications, including pediatric juvenile myelomonocytic leukemia, which received FDA approval on May 20, 2022. Oral azacitidine tablets were approved by the FDA on September 1, 2020 for continued treatment of adults with acute myeloid leukemia who achieved complete remission or complete remission with incomplete blood count recovery following intensive induction chemotherapy and cannot complete intensive curative therapy. In the European Union, azacitidine has been authorised since December 17, 2008 for similar hematologic conditions, including myelodysplastic syndromes and acute leukemias with defined marrow criteria under EMA assessments and marketing authorisations.
Uses
Azacitidine is indicated for adult patients with myelodysplastic syndromes, including intermediate‑2 and high‑risk disease categories, chronic myelomonocytic leukemia with specified blast counts, and acute myeloid leukemia with multilineage dysplasia or defined blast percentages. The oral formulation is indicated for continued treatment of acute myeloid leukemia in adults who have achieved remission after intensive induction but are not eligible to complete consolidation therapy. Azacitidine is typically administered as part of structured cycles and may be combined with other agents or used in sequence with targeted therapies where clinically appropriate, with therapy tailored to disease subtype, patient age, and treatment goals.
Administration
Azacitidine injectable powder for suspension is reconstituted and given by subcutaneous or intravenous injection under the supervision of a healthcare provider. A typical dosing schedule for the injectable form involves daily administration for seven consecutive days in a 28‑day cycle, with adjustments based on hematologic response and tolerability. Oral azacitidine tablets are administered once daily on a defined schedule, with cycles structured to balance efficacy and toxicity. Treatment continues for a minimum number of cycles and may be extended based on ongoing clinical benefit. Baseline hematologic and organ function assessments guide initial dosing, and blood counts are monitored frequently prior to each cycle to manage cytopenias and adjust dosing as needed.
Side Effects
Commonly observed side effects of azacitidine include nausea, vomiting, diarrhea, constipation, low blood cell counts such as anemia and neutropenia, fatigue, dizziness, headache, injection site reactions, fever, chills, loss of appetite, and bone pain. The frequency and severity of these effects vary among patients, and many side effects are manageable with supportive care and monitoring by a healthcare professional.
Warnings
Serious adverse events associated with azacitidine include profound bone marrow suppression leading to severe neutropenia, anemia, and thrombocytopenia, increasing the risk of serious infections, bleeding, and sepsis. Hepatic and renal dysfunctions may occur and require close monitoring of liver and kidney function during therapy. Hypersensitivity reactions including skin rash and allergic manifestations can occur. Because of the cytotoxic and epigenetic effects, azacitidine is contraindicated in patients with known hypersensitivity to the drug and requires careful evaluation before use in those with advanced hepatic tumors. Effective contraception is recommended due to potential teratogenic risks.
Precautions
Before initiating azacitidine, baseline complete blood counts, liver function tests, and renal assessments are necessary to establish organ function and hematologic status. Careful monitoring of hematologic parameters prior to each cycle is essential to identify cytopenias and guide dose adjustments. Precautions are warranted in patients with pre‑existing liver or kidney disease and in those at high risk for infections or bleeding. Concomitant use of other myelosuppressive agents may exacerbate cytopenias and should be considered carefully. Live vaccines should be avoided due to immunosuppressive effects.
Expert Tips
Patient selection for azacitidine therapy involves confirmation of hematologic malignancy subtype and assessment of baseline hematologic and organ function. Regular monitoring of complete blood counts and organ panels is critical to anticipate and manage cytopenias and toxicities. Patients should be counselled on signs of infection, bleeding, and gastrointestinal symptoms requiring prompt medical attention. Supportive care measures, including growth factor support and antiemetics, may improve tolerability. Coordination of therapy cycles, dose modifications for adverse effects, and integration with other hematologic treatments enhance patient outcomes. Clear communication about treatment schedules, duration, and monitoring requirements ensures continuity of care.